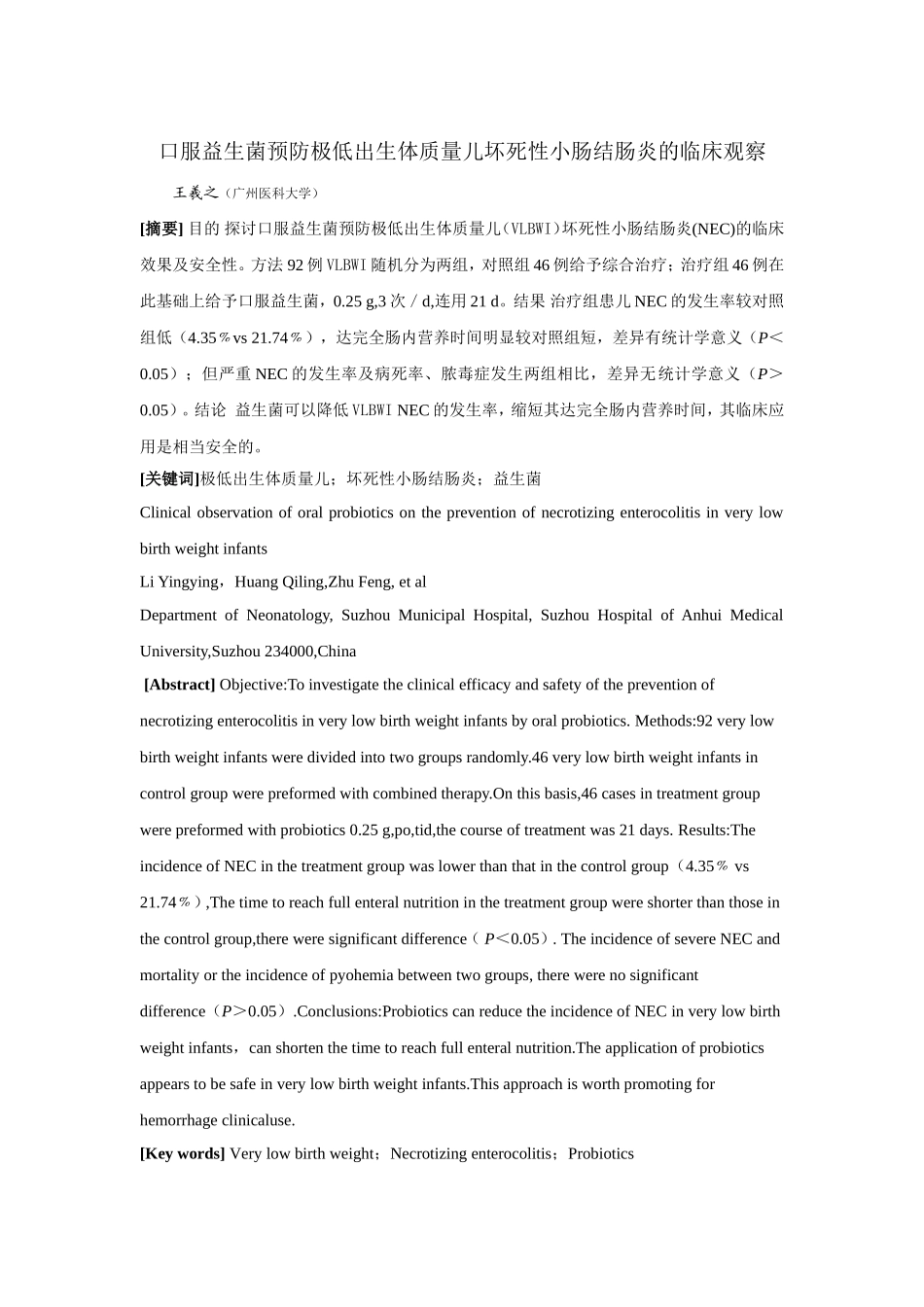
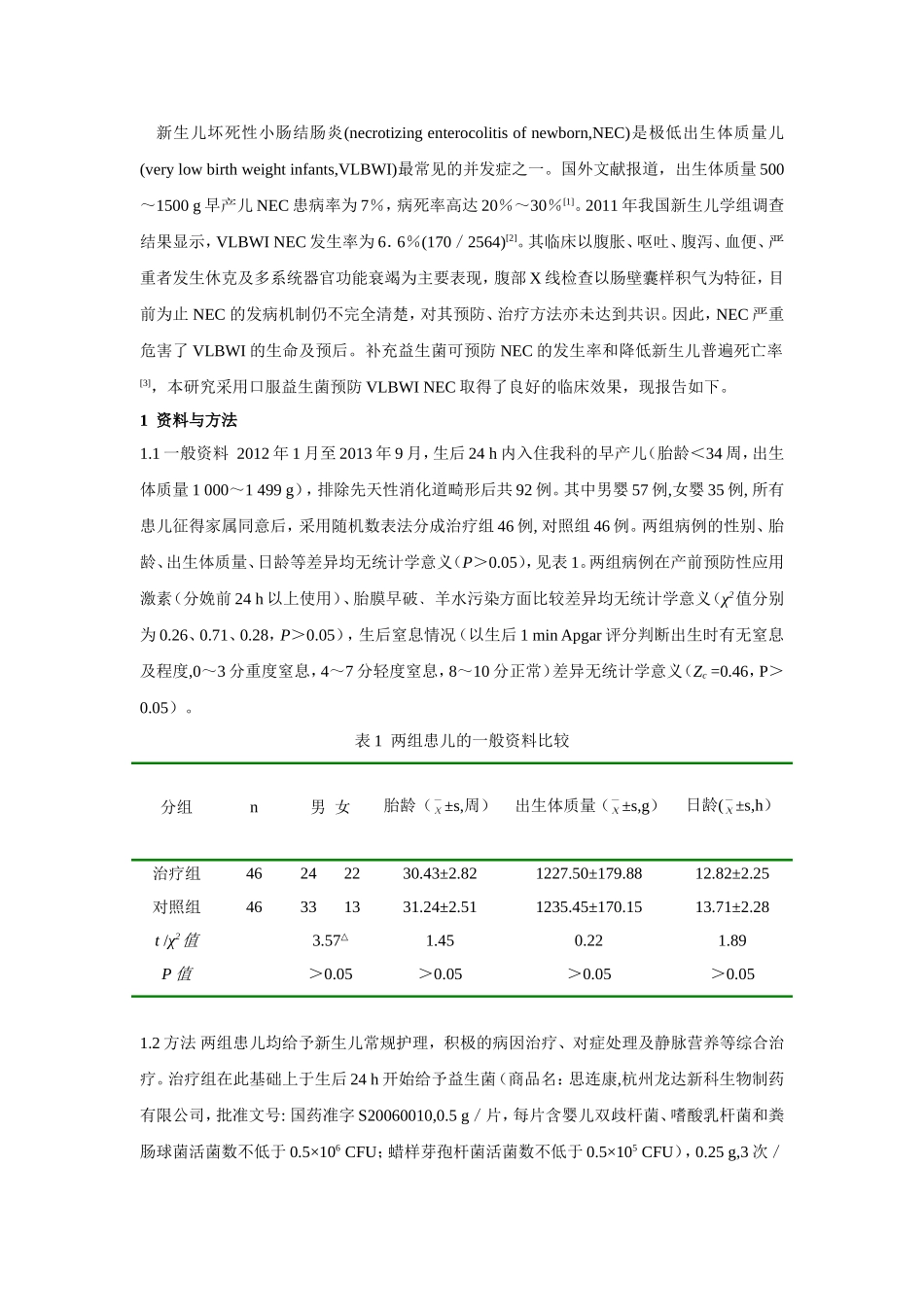
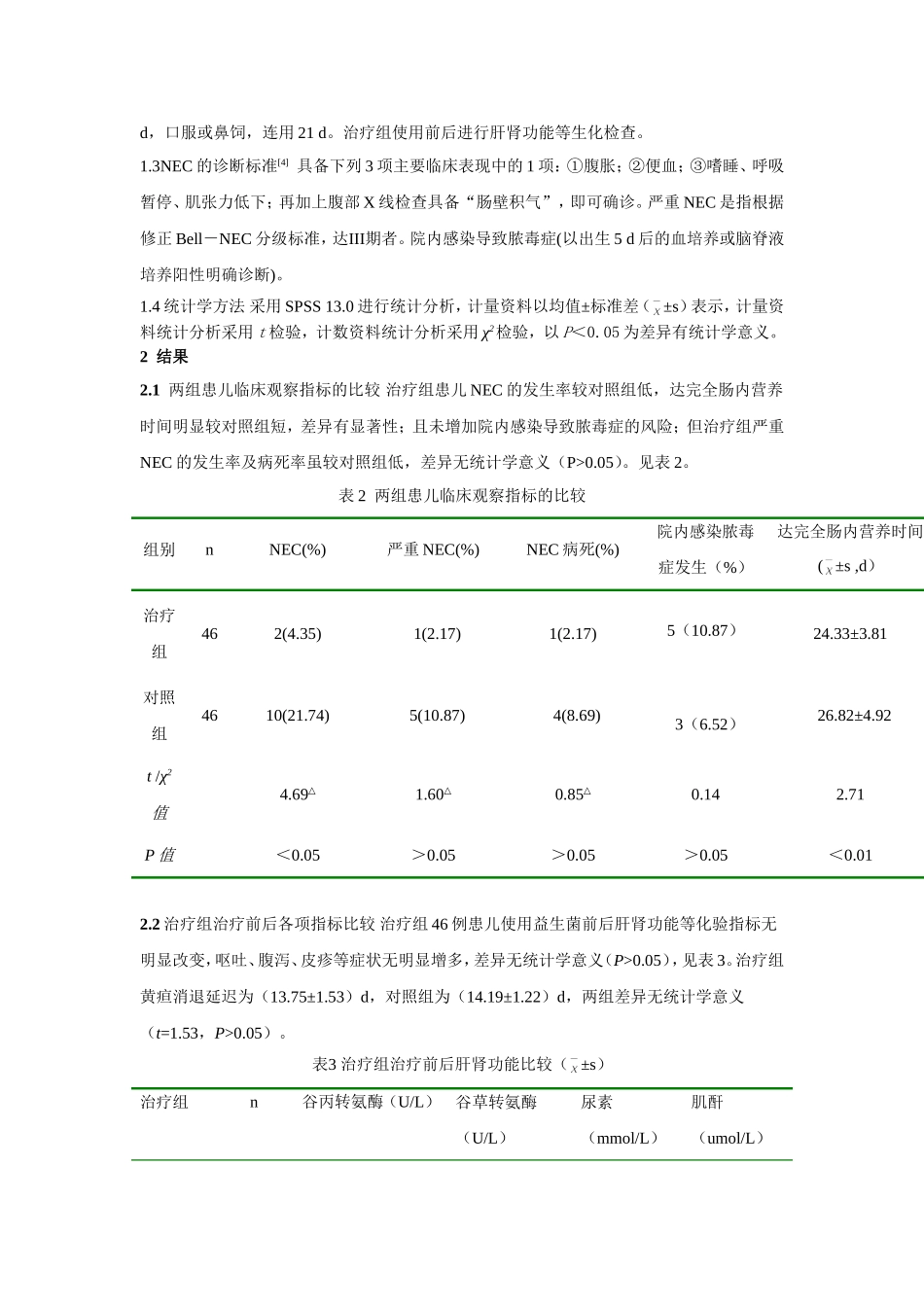
口服益生菌预防极低出生体质量儿坏死性小肠结肠炎的临床观察王羲之(广州医科大学)[摘要]目的探讨口服益生菌预防极低出生体质量儿(VLBWI)坏死性小肠结肠炎(NEC)的临床效果及安全性。方法92例VLBWI随机分为两组,对照组46例给予综合治疗;治疗组46例在此基础上给予口服益生菌,0.25g,3次/d,连用21d。结果治疗组患儿NEC的发生率较对照组低(4.35﹪vs21.74﹪),达完全肠内营养时间明显较对照组短,差异有统计学意义(P<0.05);但严重NEC的发生率及病死率、脓毒症发生两组相比,差异无统计学意义(P>0.05)。结论益生菌可以降低VLBWINEC的发生率,缩短其达完全肠内营养时间,其临床应用是相当安全的。[关键词]极低出生体质量儿;坏死性小肠结肠炎;益生菌ClinicalobservationoforalprobioticsonthepreventionofnecrotizingenterocolitisinverylowbirthweightinfantsLiYingying,HuangQiling,ZhuFeng,etalDepartmentofNeonatology,SuzhouMunicipalHospital,SuzhouHospitalofAnhuiMedicalUniversity,Suzhou234000,China[Abstract]Objective:Toinvestigatetheclinicalefficacyandsafetyofthepreventionofnecrotizingenterocolitisinverylowbirthweightinfantsbyoralprobiotics.Methods:92verylowbirthweightinfantsweredividedintotwogroupsrandomly.46verylowbirthweightinfantsincontrolgroupwerepreformedwithcombinedtherapy.Onthisbasis,46casesintreatmentgroupwerepreformedwithprobiotics0.25g,po,tid,thecourseoftreatmentwas21days.Results:TheincidenceofNECinthetreatmentgroupwaslowerthanthatinthecontrolgroup(4.35﹪vs21.74﹪),Thetimetoreachfullenteralnutritioninthetreatmentgroupwereshorterthanthoseinthecontrolgroup,thereweresignificantdifference(P<0.05).TheincidenceofsevereNECandmortalityortheincidenceofpyohemiabetweentwogroups,therewerenosignificantdifference(P>0.05).Conclusions:ProbioticscanreducetheincidenceofNECinverylowbirthweightinfants,canshortenthetimetoreachfullenteralnutrition.Theapplicationofprobioticsappearstobesafeinverylowbirthweightinfants.Thisapproachisworthpromotingforhemorrhageclinicaluse.[Keywords]Verylowbirthweight;Necrotizingenterocolitis;Probiotics新生儿坏死性小肠结肠炎(necrotizingenterocolitisofnewborn,NEC)是极低出生体质量儿(verylowbirthweightinfants,VLBWI)最常见的并发症之一。国外文献报道,出生体质量500~1500g早产儿NEC患病率为7%,病死率高达20%~30%[1]。2011年我国新生儿学组调查结果显示,VLBWINEC发生率为6.6%(170/2564)[2]。其临床以腹胀、呕吐、腹泻、血便、严重者发生休克及多系统器官功能衰竭为主要表现,腹部X线检查以肠壁囊样积气为特征,目前为止NEC的发病机制仍不完全清楚,对其预防、治疗方法亦未达到共识。因此,NEC严重危害了VLBWI的生命及预后。补充益生菌可预防NEC的发生率和降低新生儿普遍死亡率[3],本研究采用口服益生菌预防VLBWINEC取得了良好的临床效果,现报告如下。1资料与方法1.1一般资料2012年1月至2013年9月,生后24h内入住我科的早产儿(胎龄<34周,出生体质量1000~1499g),排除先天性消化道畸形后共92例。其中男婴57例,女婴35例,所有患儿征得家属同意后,采用随机数表法分成治疗组46例,对照组46例。两组病例的性别、胎龄、出生体质量、日龄等差异均无统计学意义(P>0.05),见表1。两组病例在产前预防性应用激素(分娩前24h以上使用)、胎膜早破﹑羊水污染方面比较差异均无统计学意义(χ2值分别为0.26、0.71、0.28,P>0.05),生后窒息情况(以生后1minApgar评分判断出生时有无窒息及程度,0~3分重度窒息,4~7分轻度窒息,8~10分正常)差异无统计学意义(Zc=0.46,P>0.05)。表1两组患儿的一般资料比较分组n男女胎龄(±s,周)出生体质量(±s,g)日龄(±s,h)治疗组46242230.43±2.821227.50±179.8812.82±2.25对照组46331331.24±2.511235.45±170.1513.71±2.28t/χ2值3.57△1.450.221.89P值>0.05>0.05>...