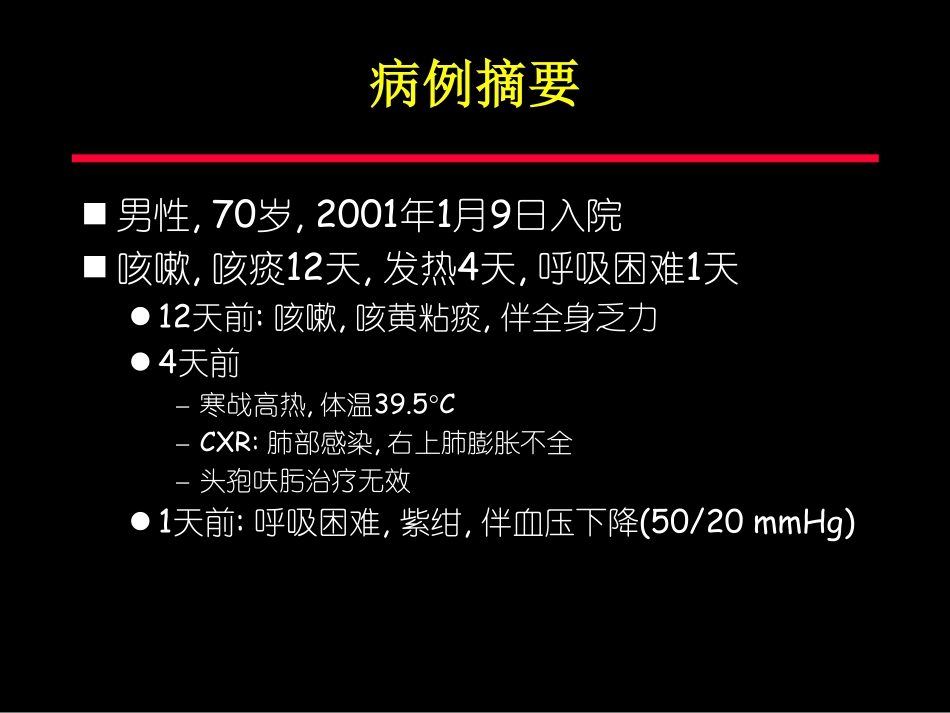
8thRespiratorySupportUpdateOctober23,2008ARDS的机械通气北京协和医院杜斌病例摘要男性,70岁,2001年1月9日入院咳嗽,咳痰12天,发热4天,呼吸困难1天12天前:咳嗽,咳黄粘痰,伴全身乏力4天前–寒战高热,体温39.5°C–CXR:肺部感染,右上肺膨胀不全–头孢呋肟治疗无效1天前:呼吸困难,紫绀,伴血压下降(50/20mmHg)病例摘要入ICU时BT37.2°CHR130bpmBP84/40mmHg(DA10µg/kg/min)SpO278%双肺散在湿罗音病例摘要呼吸功能支持(SIMV+PSV)FiO2100%PEEP10cmH2OSpO292%循环支持羟基淀粉500ml扩容无效DA13µg/kg/min–NE1.2µg/kg/minBP110/70mmHg病例摘要ARDS的机械通气保护性通气策略小潮气量适当的PEEPGirardTD,BernardGR.MechanicalVentilationinARDS:AState-of-the-ArtReview.Chest2007;131:921-929ARDS肺的形态学FRCandEELVreductioninARDSptsFromL.Puybasset,etal.Regionaldistributionofgasandtissueinacuterespiratorydistresssyndrome.I.Consequencesforlungmorphology.IntensiveCareMed2000;26:857-69.ARDS肺的形态学“婴儿肺”的概念保持通气的肺仅相当于正常肺的20-30%ARDS患者肺容积的减少并不意味着胸腔内容积的减少,仅是气体被组织所替代GattinoniL,etal.Relationshipsbetweenlungcomputedtomographicdensity,gasexchangeandPEEPinacuterespiratoryfailure.Anesthesiology1988;69:824-32.ARDS健康志愿者总CT值(HU)-256±21-654±8组织容积(ml/m2BSA)31.6±1.716.7±0.8气体容积(ml/m2BSA)11.5±1.232.2±1.8胸腔内容积(ml/m2BSA)43.0±2.349.0±2.5ARDS:机械通气的设置主要目标维持血气水平正常氧气二氧化碳通过给予超过生理水平的潮气量,且不限制气道压力呼吸机设置PEEP10.9±4.2cmH2OVt11.5±2.2ml/kgRR16.8±9bpmPIP39.4±8.6cmH2O机械通气相关性肺损伤(VALI)TobinMJ.Advancesinmechanicalventilation.NEnglJMed2001;344:1986-1996VALI:动物试验证据DreyfussDP.AJRCCM1988;137:1159VALI:临床试验证据ARDS潮气量的选择:临床试验患者数潮气量病死率作者小潮气量对照小潮气量对照小潮气量对照P值Amato29246.1±0.211.9±0.5†3871<0.001Stewart60607.2±0.810.6±0.2‡50470.72Brochard58587.2±0.210.4±0.2§47380.38Brower26267.3±0.110.2±0.1¶50460.60ARDSnet4324296.3±0.111.7±0.1¶31400.007†measuredbodyweight;‡idealbodyweight=25x[(heightinmeters)2];§Dryweightmeasuredweightminusestimatedweightgainfromsaltandwaterretention;¶Predictedbodyweight50(formales)or45.5(forfemales)+2.3[(heightininches)-60]ARDSNetworkLowVTTrial满足ALI/ARDS诊断标准<36hr呼吸机设置容量辅助控制通气模式潮气量:6vs.12ml/kgPBWPplat≤30vs.≤50cmH2ORR6-35bpm以使pH达到7.3–7.45I/E比:1.1–1.3氧合指标:PaO255–80mmHg/SpO288–95%在第四次中期分析后试验终止(疗效分析n=861;组间病死率差异p=0.005)ARDSNetwork.NEnglJMed.2000.ARDSNetwork:小VT改善病死率1.00.90.80.70.60.50.40.30.20.10.0180160140120100806040200ProportionofPatientsDaysafterRandomizationLowertidalvolumesSurvivalDischargeTraditionaltidalvaluesSurvivalDischargeARDSNetwork.NEnglJMed.2000.ARDSNetwork:主要预后指标小Vt传统VtP值住院病死率(%)31.039.80.007第28天时自主呼吸(%)65.755.0<0.001前28天内脱离呼吸机天数12±1110±110.007前28天内气压伤(%)10110.43前28天内无肺外器官衰竭天数15±1112±110.006ARDSNetwork.NEnglJMed.2000.无器官功能衰竭天数07142128RenalCoagulationCardiovascularHepaticCNSPulmonaryDays****=6ml/kg=12ml/kgTheAcuteRespiratoryDistressSyndromeNetwork:Ventilationwithlowertidalvolumesascomparedwithtraditionaltidalvolumesforacutelunginjuryandtheacuterespiratorydistresssyndrome.NEnglJMed2000;342:1301-1308ARDSNetwork:其他发现在ALI/ARDS患者,6ml/kgPBW潮气量通气策略可导致:小VT组(6ml/kg)PaO2/FiO2较低较高的RR防止CO2潴留对支持治疗的需求没有...