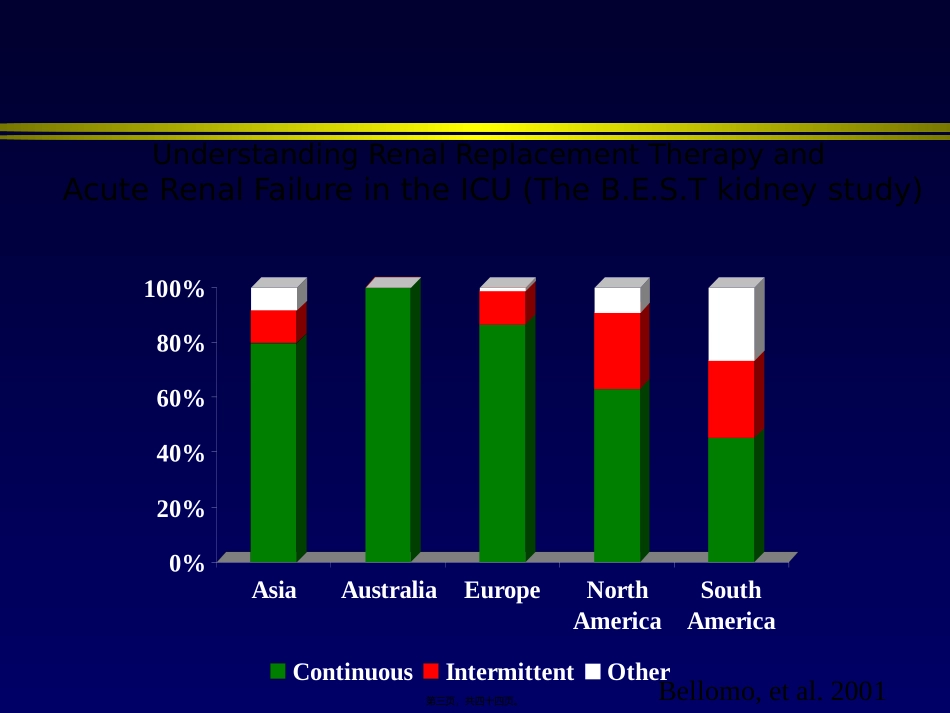
邱海波东南大学附属中大医院ICU东南大学急诊与危重医学研究所第一页,共四十四页。2.EarlyvslateCRRT3.Highvsnormalflow4.Possiblewaystoincreasemediatorsclearance第二页,共四十四页。0%20%40%60%80%100%AsiaAustraliaEuropeNorthAmericaSouthAmericaContinuousIntermittentOtherBellomo,etal.2001UnderstandingRenalReplacementTherapyandAcuteRenalFailureintheICU(TheB.E.S.Tkidneystudy)第三页,共四十四页。•Retrospectivecohortstudy•PatswithARFandrequireddialysisbetweenApril1,1996,andMarch31,1999•2ICUinCanada.•N=261CRRTIHDPAPACHEII2725.10.10BaselineSCr1361800.002MAPBeforeRRT74.787.2<0.001HospMortality71.9%42.2%<0.01Renalrecoveryinhosp80.0%62.5%0.06DurationofRRT14.7d14.5d0.91Costperweek(Can$)3486-51171341Survivor(Costpery)No-RRTRRT$11,192$73,273CritCareMed2003;31:449–455第四页,共四十四页。ICURRTn=116RRTforoverdosen=7Pre-existingCRFn=16ICURRTforARF/MOFn=66InitialCRRTn=66InitialIHDn=28JackaMJ,IvancinovaX,GibneyRTN.CanJAnaesth2005;52:327-332第五页,共四十四页。•Munnsetal观察危重急性肾衰竭患者IHDCRRT•CCr下降25%7%•尿量下降50%10%•钠排泄分数下降46%12%肾功能下降的原因:IHD平均动脉压下降,导致肾脏低灌注,加重肾脏缺血性损伤,延迟急性肾衰竭肾功能的恢复第六页,共四十四页。•160patswithARF:Dailyvsevery-other-dayIHD•Mean–Daily:1.2±0.5L–Every-other-day:3.5±0.3L(P<0.001).•occurredin–Daily:5±2%–Every-other-day:25±5%(P<0.001)•––NEnglJMed2002;346:305-310第七页,共四十四页。RRTdoseP=NS•EffectsofdifferentdosesinCVVHonoutcomesofARF:AprospectiveRCT20ml/h/kg35/ml/kg/h45ml/kg/h95%92%90%N=425Survival第八页,共四十四页。onreturnofrenalfunction第九页,共四十四页。Swzrtz.RD.ComparingcontinuousHFwithHDinpatientswithsevereARFMehti.RL.CollaborativeGroupforTreatmentofARFinICU:ARCTofcontinuousversusIHDforARF.KellumJA.ContinuousversusintermittentRRT.Ameta-analysis.ThereisnoconclusiveevidencetosupportthesuperiorityofCRRTvsIHD.Bothtechniquesarecomplimentary第十页,共四十四页。Qualityscore5:definitelyequal第十一页,共四十四页。Hospitalmortality:CRRTwasassociatedwithareducedriskofhospitaldeathinthesixstudiesinwhichbaselineseverityofillnesswassimilarRR0.48,0.34–0.69,p<0.0005IntensiveCareMed,2002,28:29-37第十二页,共四十四页。3.Highvsnormalflow4.Possiblewaystoincreasemediatorsclearance第十三页,共四十四页。•1989-1997:100例创伤后ARF•早期-后期的临界:BUN60mg/dl•两组病人创伤评分、GCS、发生休克的比例、年龄、性别和创伤分布均无差异GettingsLG.IntensiveCareMed,1999,25:805-813第十四页,共四十四页。生存率-明显差异GettingsLG.IntensiveCareMed,1999,25:805-813第十五页,共四十四页。•RCT(n=106)•Oliguria(<30cc/hr)refractorytohigh-dosefurosemide(500mgover6hrs)•Randomizedto3groups:–Early(<12h)high-volumehemofiltration(n=35;72-96L/24h)–Early(<12h)low-volumehemofiltration(n=35;24-36L/24h)–Latelow-volumehemofiltration(n=36;24-36L/24h)Boumanetal.CritCareMed30:2205-2211,2002第十六页,共四十四页。BoumanCS,etal.CriticalCareMed2002;30:2205-221174.3%68.8%75.0%0%20%40%60%80%100%28-DaySurvivalLV-LateLV-EarlyHV-EarlyTreatmentGroupn=35SOFA10.3±2.8n=36SOFA10.6±1.9n=35SOFA10.1±2.2第十七页,共四十四页。4.Possiblewaystoincreasemediatorsclearance第十八页,共四十四页。•EffectsofdifferentdosesinCVVHonoutcomesofARF:AprospectiveRCT20ml/h/kg35/ml/kg/h45ml/kg/h41%57%58%N=425Survival第十九页,共四十四页。5919ICUadmissionsOliguricARFN=248Non-oliguricARFN=130NotrandomizedinstudyN=142RandomizedInstudyN-106EHVn=35ELVn=35LLVn=36Hemof...