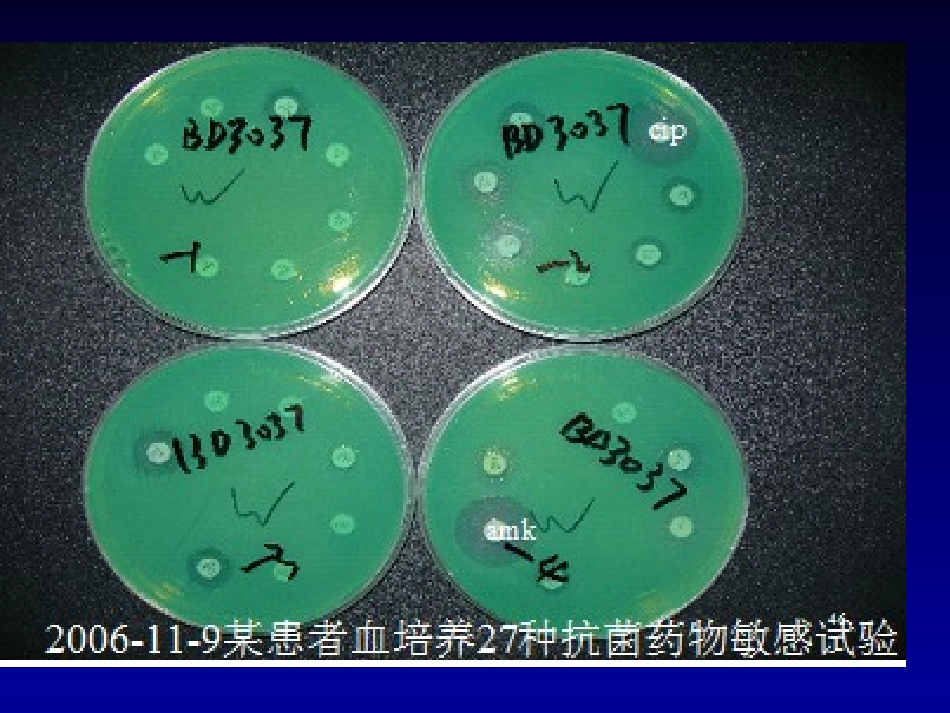
1提高感染疾病的诊治水平-----关注CLSI血培养指南王瑶北京协和医院检验科临床微生物专业组MakeempiricalMakeempiricaltherapymoretherapymoreeffectiveeffectivePatient?Etiology?Resistance?cipamk全球关注的多重耐药菌•产ESBL的肠杆菌科菌•产KPC的肠杆菌科菌•MRSA•VRE•MDRPA•CRABAPUMCH痰标本前10位的菌株OrganismNumber%Acinetobacterbaumannii45521Pseudomonasaeruginosa36416Staphy.aureus26112Kleb.pneumoniae1718Candidaalbicans1436Escherichiacoli1065Steno.maltophilia1025Enterobactercloacae583Haemophilusinfluenzae412Enterococcusfaecalis382呼吸道痰标本分离的471株鲍曼不动杆菌的耐药性分析Antibioticname%R%I%SMinocycline31.824.843.3Cefoperazone/Sulbactam49.925.924.2Imipenem69.31.928.8Meropenem72.40.826.8Levofloxacin73.36.420.3Ampicillin/Sulbactam75.23.921Amikacin77.31.321.4Cefepime77.92.519.5Piperacillin/Tazobactam78.15.116.8Ciprofloxacin800.619.4Trimethoprim/Sulfamethoxazole80.30.619Ceftazidime80.68.111.3PUMCH:痰涂片染色镜检PUMCH尿液标本前10位的菌株OrganismNum.%Escherichiacoli20834Enterococcusfaecalis6310Pseudomonasaeruginosa417Klebpneumoniae396Enterococcusfaecium335Candidaalbicans264Acinetobacterbaumannii203Staphylococcus,coagulasenegative193Staphylococcusaureus173Torulopsis(Cand.)glabrata142尿路感染分离的215株大肠杆菌的耐药性Antibioticname%R%I%SImipenem0.00.0100Meropenem0.00.0100Ertapenem0.50.099.5Piperacillin/Tazobactam3.34.792.1Cefoperazone/Sulbactam5.618.775.7Minocycline45.31638.7Cefepime60.50.039.5Cefotaxime60.61.438.0Ceftriaxone60.70.039.3Ceftazidime60.90.039.1Trimethoprim/Sulfamethoxazole73.32.424.3Levofloxacin77.63.718.7Ciprofloxacin81.40.917.7PUMCH血流感染前10位的菌株OrganismNum.%Staphy.coagulasenegative17225Escherichiacoli10215Acinetobacterbaumannii538Staphylococcusaureus416Enterococcusfaecium396Pseudomonasaeruginosa355Enterococcusfaecalis325Klebsiellapneumoniae325Candidaalbicans122Enterobactercloacae81PUMCH插管前10位的菌株OrganismNum%Staphy.,co.negative1521Escherichiacoli1014Acinetobacterbaumannii710Staphylococcusaureus68Enterococcusfaecalis68Pseudomonasaeruginosa57Staphylococcusepidermidis46Candidaspp46Burkholderiacepacia23Klebsiellaoxytoca232010年CLSI修改了头孢菌素和单环类对肠杆菌科的BP抗菌药物纸片扩散法(mm)琼脂稀释法(μg/ml)2009年2010年2009年2010年头孢他啶R≤14S≥18R≤17S≥21S≤8R>=32S≤4R≥16头孢噻肟R≤14S≥23R≤22S≥26S≤8R>=64S≤1R≥4头孢曲松R≤13S≥21R≤19S≥23S≤8R>=64S≤1R≥4CLSI降低BPs的原因:出现新的耐药机制,用以前的BP不能可靠地检测出来使用当前的BP不能较好地预测临床反应减少执行ESBL试验的需要CLSI、FDA和EUCAST之间存在差异抗菌药物大肠埃希菌(6771-6936株)肺炎克雷伯菌(2969-3009株)产酸克雷伯菌(501-506株)奇异变形杆菌(404-410株)R%I%S%R%I%S%R%I%S%R%I%S%头孢他啶9.1684.915.74.679.77.92.889.36.30.593.2头孢他啶*15.19.175.820.36.273.510.7386.46.81.791.5头孢噻肟42.713.743.525.210.164.714.61372.515.66.977.5头孢噻肟*56.53.639.935.38.756.127.58.863.722.52.774.8头孢曲松51.24.544.3295.365.621.29.76915.86.278.1头孢曲松*55.4143.533.63.263.330.43.865.920.93.475.6备注:*:本组为采用2010新折点分析结果肠杆菌科细菌纸片扩散法新旧折点药物敏感性分布KPCKPC((KKlebsiellalebsiellappneumoniaeneumoniaeCCarbapenemase)arbapenemase)•KPCconfersresistancetoallKPCconfersresistancetoall-lactams-lactams–penicillins,penicillins,–extended-spectrumcephalosporins,extended-spectrumcephalosporins,–MonobactamsMonobactams–CarbapenemsCarbapenemsblablaKPCKPCgenelocatedonplasmid;oftenoccurswithgenelocatedon...