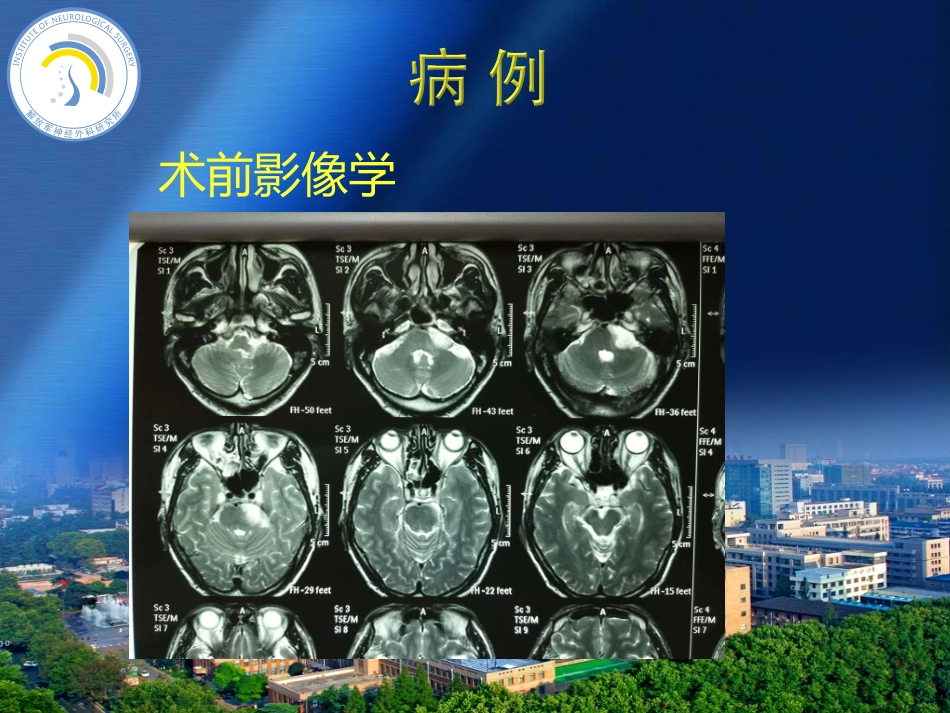
病例回顾并文献复习患者男性,60岁,因“左侧面肌痉挛半年,行走不稳1月余”入院查体:左面肌痉挛,左耳听力下降,左额感觉减退,步态不稳,余颅神经及四肢肌力、肌张力均正常病史简介术前影像学术前影像学术前影像学术前影像学术前影像学术前影像学术前影像学全麻下行开颅左侧乙状窦后入路肿瘤切除术术中见肿瘤呈灰黄色,质地软,血供丰富,肿瘤与三叉神经、面听神经及后组颅神经均有粘连,肿瘤与周围脑组织无明显边界。显微镜下肿瘤全切,手术经过顺利。手术过程术后影像学术后影像学术后影像学术后病理术后颅神经症状Primaryglioblastomaofthecerebellopontineangleinadults.JNeurosurg114:1288–1293,2011Cerebellopontineanglepilocyticastrocytomamimickingacousticschwannoma.Neuroradiology41:949–950,1999Cerebellopontineanglepilocyticastrocytomamimickingacousticschwannoma.Neuroradiology41:949–950,1999Cranialnerverootentryzoneprimarycerebellopontineanglegliomas:arareandpoorlyrecognizedsubsetofextraparenchymaltumors.JNeu-rooncol49:205–212,2000Cranialnerverootentryzoneprimarycerebellopontineanglegliomas:arareandpoorlyrecognizedsubsetofextraparenchymaltumors.JNeu-rooncol49:205–212,2000Cranialnerverootentryzoneprimarycerebellopontineanglegliomas:arareandpoorlyrecognizedsubsetofextraparenchymaltumors.JNeu-rooncol49:205–212,2000Cranialnerverootentryzoneprimarycerebellopontineanglegliomas:arareandpoorlyrecognizedsubsetofextraparenchymaltumors.JNeu-rooncol49:205–212,2000Pediatricprimarypilocyticastrocytomaofthecerebellopontineangle:acasereport.ChildsNervSyst25:247–251,2009Pediatricprimarypilocyticastrocytomaofthecerebellopontineangle:acasereport.ChildsNervSyst25:247–251,2009Pediatricprimarypilocyticastrocytomaofthecerebellopontineangle:acasereport.ChildsNervSyst25:247–251,2009Primaryglioblastomaofthecerebellopontineangleinadults.JNeurosurg114:1288–1293,2011Primaryglioblastomaofthecerebellopontineangleinadults.JNeurosurg114:1288–1293,2011CPA胶质瘤发病率Trigeminalnerverootentryzonepilocyticastrocytomainanadult:ararecaseofanextraparenchymaltumor.JNeurooncol.201097(2):285-90早期临床表现以病灶侧CN(V-XII)相关颅神经功能障碍为主,而很少伴有脑干或小脑相关症状有些此类病例甚至可出现内听道扩大征象由于肿瘤的相对恶性特征,此类患者的病程往往相对较短。本病例病程约半年,以三叉面听神经相关神经功能异常为主CPA胶质瘤临床表现现有文献报道的CPA胶质瘤大多数为低级别,以纤维型或毛细胞型星形细胞瘤为主少数病例则为高级别胶质瘤,此类病患预后差,术后生存时间<6个月CPA胶质瘤病理分型Primaryglioblastomaofthecerebellopontineangleinadults.JNeurosurg114:1288–1293,2011根据生发部位不同,分为原发型和外生型原发型:原发于CPA,与桥脑及小脑界限分明,有明确的蛛网膜间隙;发生点通常为V或VIII颅神经出脑干处外生型:由脑干及小脑向外生长,肿瘤与桥脑或小脑无明确的蛛网膜间隙CPA胶质瘤临床分型入脑干段学说异位神经胶质簇学说播散学说CPA胶质瘤起源CPA胶质瘤并无典型的影像学表现,有时易与其他常见的CPA肿瘤混淆(CASE1)有作者认为术前行DWI或PWI有助于进一步鉴别此区域内胶质瘤和其他类型肿瘤[1]也有报道认为,CPA胶质瘤患者血清中高表达的NSE、GFAP或ferritin提示胶质瘤可能(CASE4)CPA胶质瘤影像学及其他检查[1]MRimagingofglioblastomainchildren:usefulnessofdiffusion/perfusion-weightedMRIandMRspectroscopy.PediatrRadiol2003,33(12):836-842.治疗CPA胶质瘤包括开颅最大限度肿瘤切除,后续行同步放化疗,但对于高级别胶质瘤,总体效果欠佳,大部分患者仅有1年左右的生存期[1]一些临床医生认为,由于肿瘤靠近后组颅神经,同步放化疗可引发心律失常,不主张术后放化疗[2]。CPA胶质瘤治疗[1]Glioblastomamultiforme:areviewoftherapeutictargets.ExpertOpinTherTargets2009,13(6):701-718.[2]Primaryglioblastomaofthecerebellopontineangleinadults.JNeurosurg2011,114(5):1288-1293.CAP胶质瘤发病率极低无特征性临床表现影像学表现,易与其他CPA肿瘤混淆临床分型根据生发部位不同,分为原发型和外生型原发型通常起源点为V或者VIII入脑干段对于术后是否放化疗有争议